A giant, lengthy study of screening mammography concludes that the test offers no benefit to women regardless of age… and may do more harm than good. In a 25 year follow up of nearly 90,000 Canadian women randomized to get annual mammograms for five years or to receive usual care (but no mammograms). There was no difference in deaths from breast cancer.
How can this be? After all, over that same period, we have seen five-year survival rates rise and deaths from breast cancer drop (data from SEER).
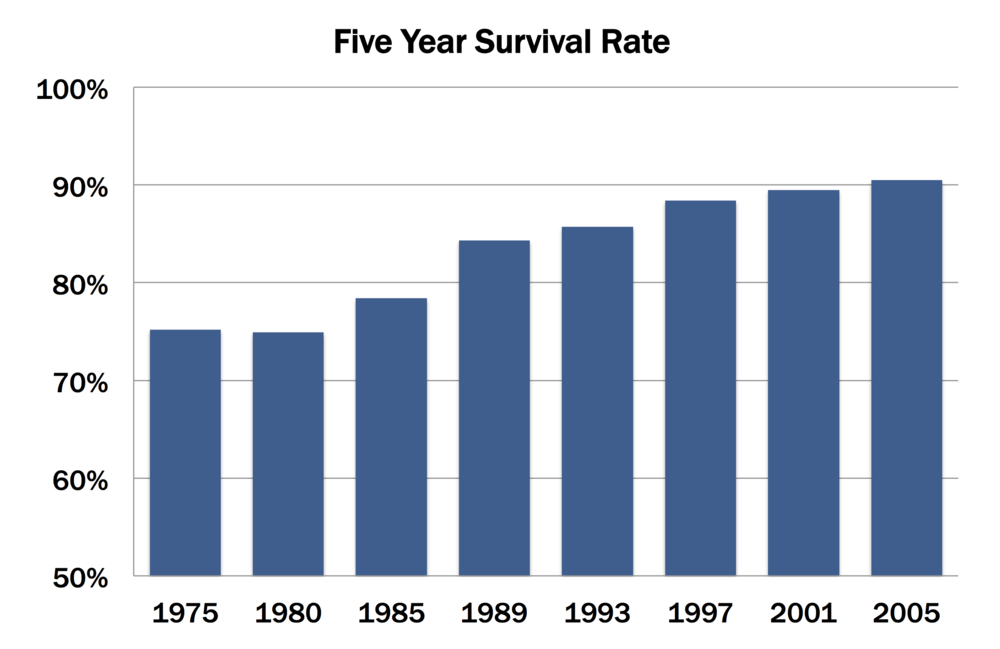 Five-year survival rates after diagnosis with breast cancer have rise dramatically since 1980…
Five-year survival rates after diagnosis with breast cancer have rise dramatically since 1980…
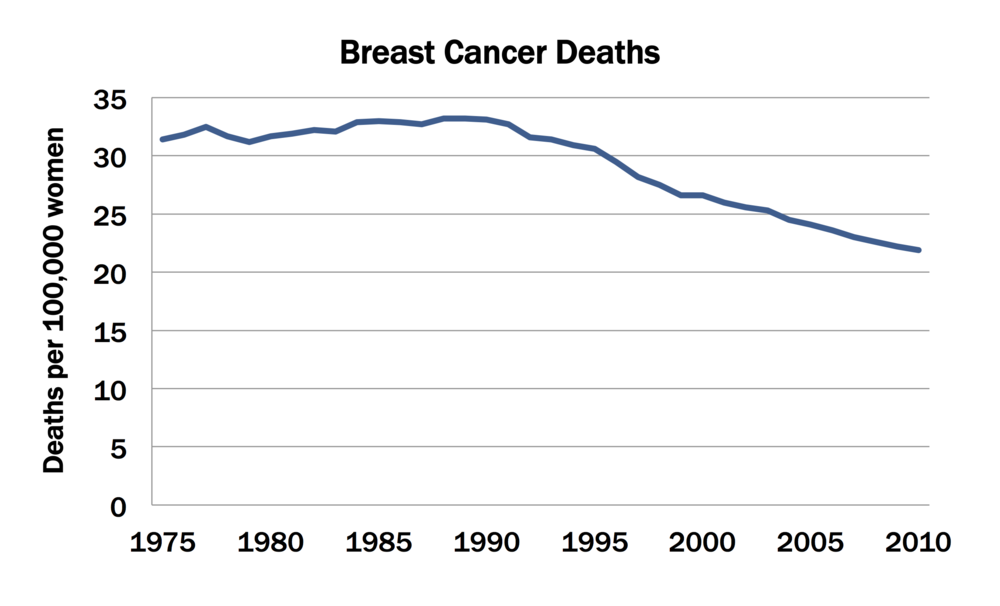 … while deaths from breast cancer have dropped steeply.
… while deaths from breast cancer have dropped steeply.
Many folks attribute the gains in breast cancer survival to the use of mammograms. After all, intuition tells us that screening allows doctors to “catch” cancers when they are smaller and more treatable… and, in fact, that’s the rationale for screening mammograms.
And when you look at data in charts like those above, you come to the conclusion that screening really works. In fact, unless you do a randomized controlled trial (which we’ll get to in minute), nearly every indication from ANY screening test is that it improves outcomes. Here’s why.
First, let’s say you measure how long patients survive from the time their cancer is detected until they die. If the screening test finds tumors before they would otherwise become apparent, the time from diagnosis to death must increase… even if early detection doesn’t change the course of the disease one bit. Survival from diagnosis goes up, but not because you’ve slowed the disease. It’s just because you made the diagnosis earlier in the course of the disease. This is known as “lead time” bias.
Another measure that cancer folks use is a the grade of the tumor at the time of detection. “Grade” refers to how aggressive the tumor is. When you look at the mix of tumors picked up at screening, the average grade tends to be lower (i.e., more favorable) than that of tumors picked up when they become clinically apparent. This seems like a really good thing: you’re finding tumors that slower growing, and thus easier to treat.
But in fact, all that’s happening is that you’re missing the fastest growing (i.e., higher grade) tumors – they are the ones that are emerging in between screenings. (They’re also the ones that are most likely to lead to bad outcome.) This is known as “length” bias. The slower growing the tumor, the more likely it is to be picked up during screening. And ironically, those slower growing tumors may not need to be treated at all.
This is precisely how our intuition fails us when it comes to screening mammograms. The basic rationale makes sense (catch and treat the disease early), and the observational data support that the rationale is true. The problem is, at least in the case of mammograms, data from randomized controlled trials strongly suggest that screening does little if anything. (Note: There is one thing about which we can be absolutely certain: screening mammograms lead to a lot of anxiety and additional work up. The BMJ paper reports that about one in five of the women screened with invasive cancers were overdiagnosed: they learned early about their cancers, possibly pursued treatment, and had absolutely nothing to show for it.)
As noted previously, the only way to really know whether screening tests work is to use randomized controlled trials. With randomized controlled trials (or RCTs), subjects are randomly assigned to get the intervention (here, screening mammogram) or not. This means that the only difference between the groups is whether or not they are exposed to the intervention. Once this is done, researchers can directly compare the two groups on whatever outcome they want (e.g., deaths from breast cancer).
This is the approach the researchers used in the BMJ study. In fact, when they published their results 12 years ago (again, showing no benefit for screening mammograms), proponents of screening argued that their follow up was too short — that the benefits would emerge down the line. The researchers now have 25 years of follow up, and there’s no indication that the purported benefit will emerge.
We’re left with one mystery. Why did deaths from breast cancer drop? There really were fewer deaths, and we can’t explain that away with lead time and length biases. The answer is very likely due to improvements in the treatment of breast cancer later in the course of the disease. Drugs like tamoxifen have made serious inroads in the successful treatment of breast cancer. And the evidence now suggests that we would have enjoyed those gains whether or not we’d aggressively pushed screening mammograms.
This discussion is far from over. Emotions will run high, and beliefs will remain entrenched. Health plans will be caught between relying on the best available science and looking like they don’t care about women’s health. Ditto policymakers.
And don’t be surprised if screening proponents now tell us that mammogram technology has vastly improved since the 1980s, and that this study – with the longer follow-up they demanded – is no longer relevant. Sometimes intuition is tough to set aside even in the face of overwhelming evidence.